The concept of fetal programming has emerged as a groundbreaking framework in clinical medicine, reshaping our understanding of how early developmental environments influence lifelong health. This theory posits that the uterine environment—shaped by maternal nutrition, stress, and other factors—can "program" the fetus's physiology in ways that manifest as disease susceptibility decades later. Clinicians are now translating these insights into practical interventions, though the field remains ripe with unanswered questions and ethical considerations.
From Theory to Examination Room
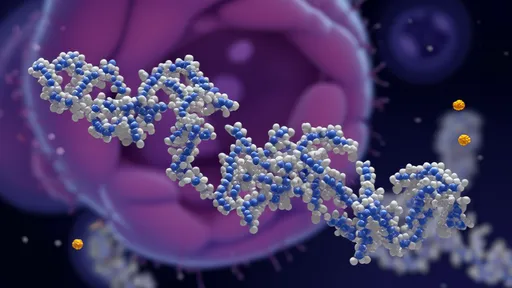
The leap from fetal programming theory to clinical practice hasn’t been straightforward. Unlike genetic testing, which offers clear biomarkers, programming effects operate through epigenetic modifications, subtle metabolic shifts, and organ system adaptations that aren’t always detectable at birth. Pioneering obstetricians now incorporate maternal dietary assessments and stress evaluations into routine prenatal care, not just for immediate pregnancy outcomes but for their potential decades-long consequences. A mother’s micronutrient deficiencies or elevated cortisol levels, once considered marginal concerns, now warrant closer scrutiny.
Neonatology units have become unexpected testing grounds for programming hypotheses. Researchers tracking preterm infants—a population exposed to abrupt nutritional and environmental transitions—find these children show distinct metabolic patterns compared to full-term peers. Some NICUs now tailor early nutritional regimens based on this data, though the long-term outcomes remain to be seen. The delicate balance between supporting rapid growth (critical for preterm survival) and avoiding overnutrition (a potential programming trigger for later obesity) illustrates the nuanced decisions clinicians face.
The Two-Generation Approach
Forward-thinking practices adopt what’s termed a "two-generation" intervention model. A diabetic pregnancy clinic, for instance, doesn’t just manage maternal glucose to prevent macrosomia; it educates mothers about how glycemic control might reduce their child’s own diabetes risk. Pediatricians inheriting these infants monitor not just milestone achievements but subtle signs—accelerated weight gain trajectories, atypical appetite regulation—that could reflect programmed metabolic tendencies. This continuity of care across what was traditionally separate medical silos represents one of the theory’s most transformative clinical impacts.
Emerging technologies are bridging gaps between programming theory and actionable data. Advanced MRI techniques can now detect subtle differences in fetal brain development associated with maternal psychological distress. While not yet standard practice, such tools may eventually guide interventions like targeted cognitive enrichment programs for at-risk infants. Similarly, research into the placental transcriptome offers hope for identifying programming-related biomarkers that could be measured through non-invasive maternal blood tests—a potential game-changer for risk stratification.
Controversies and Cautions
Not all researchers agree on how aggressively to implement programming-based interventions. Critics argue that without large-scale longitudinal studies, some clinical adaptations may be premature. The field grapples with difficult questions: Should all pregnant women undergo detailed metabolic profiling? How do we avoid creating undue anxiety about factors only marginally within a mother’s control? The shadow of "blaming mothers" for their children’s later health problems looms large, requiring sensitive communication frameworks.
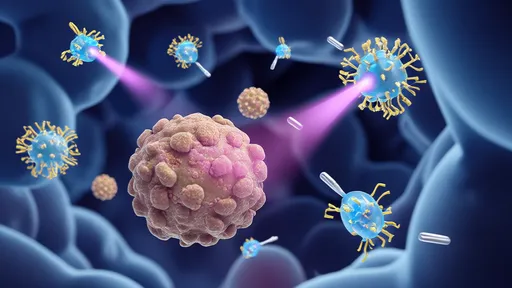
Ethical considerations multiply when discussing interventions that could alter fetal programming pathways. Experimental approaches like maternal microbiome transplantation or targeted micronutrient supplementation during critical gestational windows show promise in animal studies but raise complex risk-benefit questions in humans. Regulatory bodies struggle to balance innovation with caution, as the true outcomes of programming interventions may not be apparent for generations.
Beyond Birth: Lifespan Implications
The most profound clinical implications may lie in how fetal programming insights reshape lifelong healthcare strategies. A cardiologist evaluating a middle-aged patient with hypertension now considers not just current lifestyle factors but potential fetal origins of vascular dysfunction. Some progressive practices incorporate birth weight and maternal pregnancy history into adult disease risk assessments—a radical departure from traditional medical history-taking. This paradigm shift acknowledges that our health narratives begin not at birth, but at conception.
Nutrition science has been particularly transformed. The old adage "you are what you eat" now competes with "you are what your mother ate." Dietary recommendations for women of childbearing age increasingly emphasize not just fertility support but potential programming effects. Functional foods enriched with specific methyl donors or omega-3s are being studied for their ability to favorably influence epigenetic programming, though the market risks outpacing the evidence.
The Road Ahead
As the science matures, the clinical applications of fetal programming theory will likely become more targeted and personalized. Imagine a future where epigenetic profiling at birth guides individualized preventive healthcare plans, or where assisted reproductive technologies include programming optimization alongside genetic screening. The coming decades will test whether these theoretical possibilities can be translated into measurable improvements in population health.
What remains clear is that fetal programming has shattered the artificial divide between obstetrics and lifelong medicine. The womb is no longer seen merely as a protective capsule, but as an active architect of human biology—one that clinicians are learning to thoughtfully engage with for generations to come. This paradigm doesn’t just change pregnancy management; it redefines our very conception of disease prevention.

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025