The field of epigenetic reprogramming has emerged as a revolutionary approach in regenerative medicine and aging research, offering the tantalizing possibility of resetting cellular aging and treating age-related diseases. However, as scientists delve deeper into the mechanisms and applications of this technology, concerns about its safety profile have come to the forefront. The potential risks, ranging from unintended genomic instability to the reactivation of dormant oncogenes, demand rigorous scrutiny before clinical translation.
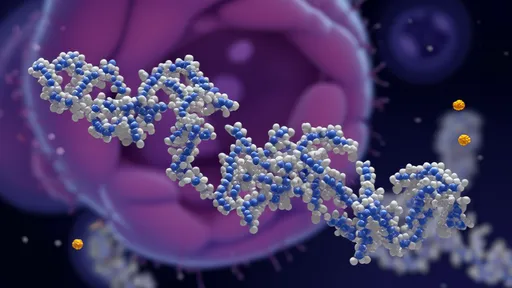
Epigenetic reprogramming, at its core, involves the modification of gene expression patterns without altering the underlying DNA sequence. Techniques such as the use of Yamanaka factors (Oct4, Sox2, Klf4, and c-Myc) have shown remarkable success in reverting differentiated cells to a pluripotent state. While this holds immense therapeutic promise, the process is not without its pitfalls. The very factors that enable cellular rejuvenation can also trigger uncontrolled proliferation or malignant transformation, raising red flags for researchers and clinicians alike.
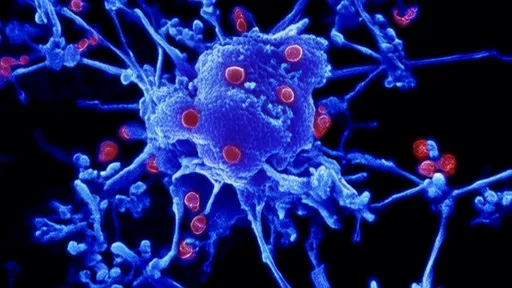
One of the most pressing safety concerns revolves around the reactivation of transposable elements. These "jumping genes," normally silenced in healthy cells, can wreak havoc if unleashed during reprogramming. Studies have documented instances where epigenetic modifiers inadvertently activated endogenous retroviruses, leading to genomic instability and cellular dysfunction. The long-term consequences of such events remain poorly understood, particularly in the context of in vivo applications where systemic effects could be far-reaching.
The duration and intensity of reprogramming stimuli present another critical safety consideration. Partial reprogramming approaches have gained traction as a potentially safer alternative to complete dedifferentiation, aiming to rejuvenate cells without erasing their identity. Yet, even these moderated protocols carry risks. The epigenetic landscape of partially reprogrammed cells may enter an unstable intermediate state, potentially predisposing them to aberrant behavior. Striking the precise balance between therapeutic benefit and safety remains an ongoing challenge.
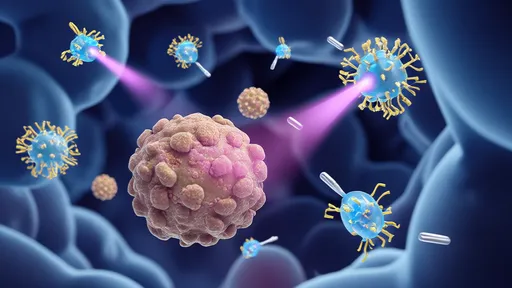
Immunogenicity represents another layer of complexity in assessing reprogramming safety. Epigenetically altered cells may express neoantigens or stress-induced ligands that mark them for immune surveillance. While this could theoretically help eliminate potentially dangerous cells, it might also trigger autoimmune reactions or graft rejection in therapeutic contexts. The interplay between reprogrammed cells and the host immune system adds yet another variable to the already complex safety equation.
Beyond cellular-level concerns, the tissue-specific effects of epigenetic reprogramming warrant careful examination. Different cell types exhibit varying susceptibility to reprogramming factors, and the same intervention might yield dramatically different outcomes across tissues. For instance, neuronal cells might respond to reprogramming stimuli differently than cardiomyocytes, potentially leading to unpredictable tissue-specific toxicities. This heterogeneity underscores the need for comprehensive preclinical testing across multiple tissue types.
The potential for off-target effects looms large in epigenetic interventions. Unlike gene editing technologies that target specific sequences, epigenetic modifiers often have broader activity profiles. Small molecule inhibitors of DNA methyltransferases or histone deacetylases, while promising as reprogramming adjuvants, may affect thousands of genomic loci simultaneously. This lack of precision increases the likelihood of unintended consequences, particularly when considering the delicate balance of epigenetic regulation in maintaining cellular homeostasis.
Long-term safety data remains conspicuously absent from the epigenetic reprogramming landscape. Most studies to date have focused on short-term outcomes, leaving questions about delayed effects unanswered. Could epigenetic reprogramming accelerate aging in certain cell populations? Might it predispose tissues to late-onset dysfunction? These unanswered questions highlight the need for extended follow-up in both animal models and, eventually, human trials.
As the field progresses, the development of safety-enhanced reprogramming strategies has become a major research focus. Approaches such as transient mRNA delivery, small molecule cocktails, and precision epigenome editing aim to mitigate risks while preserving therapeutic potential. The integration of single-cell technologies and advanced computational modeling offers new opportunities to predict and monitor safety parameters at unprecedented resolution.
The regulatory landscape for epigenetic reprogramming therapies remains in its infancy, presenting both challenges and opportunities. Current frameworks for cell and gene therapies may not adequately address the unique safety considerations of epigenetic interventions. Developing appropriate guidelines will require close collaboration between researchers, clinicians, and regulatory bodies to ensure patient safety without stifling innovation.
Ultimately, the promise of epigenetic reprogramming must be balanced against its potential perils. While the technology holds transformative potential for medicine, its safety profile will determine whether it transitions from laboratory curiosity to clinical reality. As research progresses, a nuanced understanding of risks and benefits will be essential to harness the power of epigenetic reprogramming while safeguarding patient health.

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025